When SARS Ended
When SARS Ended
The viral spell broke, and Hong Kong seemed to wake from a fever dream.
By Karl Taro Greenfeld. April 17, 2020
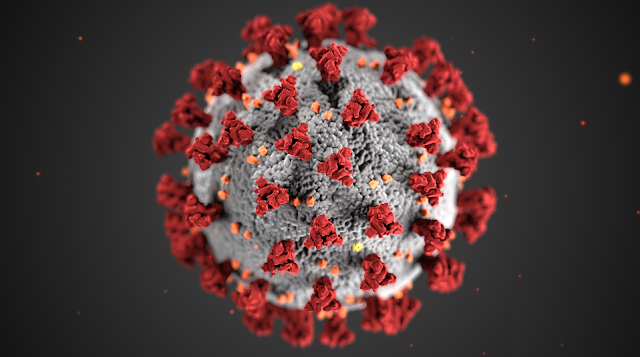
In the spring of 2003, my family and I were living in Hong Kong, in a colonial-era flat near Victoria Peak, the mountain that dominates the city’s skyline. The previous year, just to the north, a coronavirus had emerged that caused severe acute respiratory syndrome, or sars. The virus, called sars-CoV, had jumped the species barrier in a market, travelling from bats to civets to people. Its mortality rate was around ten per cent.
Initially, the Chinese government covered up the epidemic, threatening and silencing the physicians who issued warnings. Then, as the infection spread, it imposed a drastic crackdown on all social interaction. The national May Day holiday, when hundreds of millions of people travel around the country on vacation, was cancelled, and the Rolling Stones called off their concerts. Hong Kongers enacted social isolation even before it was ordered, and many expats departed, including my wife and daughters. By March, the city felt deserted. Night clubs were closed, restaurants abandoned, shopping malls desolate. The drive down Kennedy Road to Gloucester Road and then east along Hong Kong Island to my offices in Quarry Bay, usually a half-hour struggle through some of the densest traffic in the world, was now a fleet five minutes.
The New Yorker’s coronavirus news coverage and analysis are free for all readers.
For those who remember sars firsthand, the unfolding of the current covid-19 pandemic has been eerily familiar. The new coronavirus appears to have spilled over in Hubei Province, a few hundred miles north of Guangdong Province, where sars emerged; China’s decisions—the initial coverup, the cancellation of Lunar New Year celebrations, the rapid, gigantic mobilization—have echoed the past, too. (Its measures appear to be working; as of this writing, the spread of infection in mainland China has slowed dramatically.) Los Angeles, the city where I live now, looks the way Hong Kong did then. On Saturday night, I walked down to Sunset Boulevard, the city’s iconic thoroughfare, and stood in the middle of the street. The signals went from green to red to green again; no cars came. Happy cities may be happy in their own ways, but cities in the grip of disease share a common emptiness.
Hong Kong had been in crisis even before sars. In 1997, Great Britain had handed the city over to China, in an agreement known as One Country, Two Systems. After reunification, Shanghai threatened to become China’s new financial capital, and people in Hong Kong worried that they would soon be living in “just another Chinese city”; its real-estate markets began a precipitous decline, and restrictions on civil liberties threatened its nominal sovereignty. sars felt like a knockout blow to a city already reeling.
I was in Hong Kong because I edited Time Asia, an international edition of the newsweekly with a staff of sixty-two and bureaus around the region. When sars broke out, we couldn’t work from home—the Internet wasn’t good enough. Instead, we watched from our offices as the green-and-white-roofed Star Ferry boats travelled, empty, across Victoria Harbor. Each afternoon, we waited for the Hong Kong Department of Health to release its numbers. We kept a betting pool, guessing how many new cases there would be. The idea was to get close but not go over; an optimist, I always lowballed.
We were trying to make light of a reality that had become terrifying. Hong Kong’s hospital system had crashed. Hundreds of front-line health workers had been infected, most of them through so-called super-spreader events. In the first, a mainland doctor, Liu Jianlun, had treated a patient in Guangdong who would later become known as the Poison King, because of how many cases could be traced back to him. After meeting the Poison King, Liu, who was in Hong Kong for a wedding, checked into the Metropole Hotel, went shopping on Nathan Road, and then returned to the hotel, where he vomited; the next day, he admitted himself to Kwong Wah Hospital, warned the attending physicians that what he had was highly contagious, and lost consciousness, ultimately infecting a half-dozen doctors and nurses. A larger cluster of cases at Prince of Wales Hospital, originating from an airport worker who had visited the Metropole, resulted in more than a hundred hospital workers falling ill. Some of the standard treatments for patients in respiratory distress—including the use of nebulizers, humidifier-like devices that turn liquid medicine into a breathable mist—ended up spreading the virus through the wards.
These stories and others deepened our dread; the government’s obfuscation compounded it. We learned that officials had been hiding cases, moving patients out the back doors of hospitals while World Health Organization inspectors came in the front. We suspected that what we didn’t know was worse than what we did. We imagined vast wards of the infected, gasping for breath.
The Hang Seng Index, which tracks stocks listed on Hong Kong’s exchange, shed fifteen per cent of its value between January and April. After a prankster falsely suggested that the city was going to be sealed off, some A.T.M.s briefly ran out of cash. Then, as if things couldn’t get any worse, on the first of April, Leslie Cheung, the openly bisexual Cantopop crooner and actor who had starred in “Happy Together” and “Farewell My Concubine,” leapt from the twenty-fourth floor of the Mandarin Oriental Hotel. Cheung had always felt like a lucky charm for Hong Kong—a beloved and approachable celebrity we could see drinking in Lan Kwai Fong on any given night. Cheung’s death—he had suffered from depression—darkened our already dour moods.
Barely visible from my office windows was Amoy Gardens, an orange-and-beige housing complex. Nineteen buildings, each about thirty stories tall, housed about nineteen thousand people. The complex had become a notorious epicenter of the virus—the place, it was said, where sars had gone airborne. On March 14th, an infected man visited his brother’s apartment; a week later, the complex had three or four cases; the next day, six or seven more. Soon, more than sixty new cases a day were emerging at Amoy Gardens, until there were nearly three hundred and thirty, many of them in block E, where the brother’s unit was located. What was terrifying about the Amoy Gardens cluster was its banality. It looked exactly like every other housing estate in Hong Kong. As television anchors solemnly intoned over footage of the apartments, with their 7-Eleven, McDonald’s, and ParknShop downstairs, one couldn’t help but think that what was happening there could happen anywhere. (Later, it would turn out that the design of the drainage systems in the apartments had facilitated the spread of sars.)
Meanwhile, in our offices, we wore protective gear. Talked about hand washing. Kept our distance. Outside of work, we lived solitary lives. Every social event was postponed into the indefinite future. I ate dinner alone in my flat, its diamond-necklace view of the city eerily dark. My lunch each day consisted of Chicken McNuggets. I had thought it through and concluded that, from slaughter to preparation, the McNugget process was such that no nugget risked contact with potentially virus-bearing human flesh. The industrial workers wore rubber gloves and masks; the nuggets were deep-fried in boiling oil hot enough, I hoped, to render any virus inactive.
ADVERTISEMENT
At the time, many of us pinned our hopes on the “seasonality” of the virus. Infectious diseases often become more or less potent depending on the time of year; respiratory viruses—influenza in particular—are known to be seasonal. Other coronaviruses, like the ones that cause the common cold, ebb as the days lengthen and the sun rises higher in the sky. If there’s a flu season, we asked, why couldn’t there be a sars season, too?
VIDEO FROM THE NEW YORKER
Why Hong Kong’s Protests Exploded
Marc Lipsitch, a Harvard epidemiologist, has written a widely discussed blog post on the question of whether the new coronavirus—sars-CoV-2—could be seasonal. Lipsitch explains that seasonality depends on four factors: the environment (some viruses survive best in dry, cold air); human behavior (people cluster differently in summer and winter); the human immune system (in general, it’s weaker in the cold months); and the dynamics of disease more generally (an epidemic that begins in one season tends to end in another). Seasonality, in other words, isn’t just about weather. It’s a complex phenomenon, in which environmental, epidemiological, and human elements intertwine.
“Seasonality is a universal driver of almost all of our infectious diseases,” Micaela Martinez, an infectious-disease ecologist at Columbia’s Mailman School of Public Health, told me. Martinez’s research focusses on identifying the causal mechanisms behind seasonality. It’s possible, for instance, that, for certain diseases, circadian rhythms matter: because the location of some immune-system cells in the body varies depending on the time of day, longer days could change how the immune system responds to an infection. (Many of covid-19’s worst symptoms—fever, inflammation, fluid in the lungs—are the result of inappropriate immune-system responses.) Martinez stressed how much is unknown about the biology of seasonality. “I hope for seasonal decline,” she said. But, in the case of sars-CoV-2, seasonal factors could be outweighed by the scale of the outbreak and the ease with which the virus spreads.
Both sars-CoV and sars CoV-2 are RNA coronaviruses. “Fields Virology,” the standard medical-school text on the subject, notes that “coronaviruses mutate at a high frequency because of the high error frequencies of RNA polymerases.” (RNA is a single long strand; unlike double-helixed DNA, it has no second strand to check its errors.) “When you have a mutation, there tends to be a survival disadvantage for the virus,” Charles Prober, a pediatric epidemiologist at Stanford University, told me. It’s possible, therefore, to imagine that sars-CoV-2 could mutate its way into a seasonal decline. As an “optimist,” Prober said, he was hoping for such an outcome. There’s room for luck in an epidemic. It’s also possible, through bad decisions, to squander a lucky break.
We didn’t know it yet, but that week—the week of Leslie Cheung’s death—was the point of maximum hysteria and fear. In early April, while we were betting on the number of new cases and wondering about the extent of the coverup, Hong Kong passed its inflection point, with the number of new infections sinking below that of cleared cases. As April turned to May, and warmer days commenced, we looked around and realized that we were still alive.
What had actually happened? In retrospect, it seems likely that several factors converged. We had all effectively self-quarantined (or, in the case of my wife and daughters, actually departed). Schools had been closed for more than a month. Everyone in the city had been wearing surgical masks, without exception; on television, even government officials appeared in scrubs and full protective gear.
The medical system had adapted, too. Prior to sars, some hospitals had become lax, relying on antibiotics for infection control instead of maintaining disinfection as a steady state. What worked against sars, I wrote later, in my book about the outbreak, “China Syndrome,” were “Florence Nightingale-style proscriptions: protective layers of masks, goggles, gloves, galoshes, and gowns. Sealed wards. Quarantine. Ventilation. This was not Nobel Prize-winning medicine. Yet it was effective.” Modern hospital systems aren’t accustomed to swarms of critical respiratory cases. But Hong Kong’s hospitals, after becoming overwhelmed, had adjusted.
At the time, it also seemed to us that the weather played a role. Hong Kong in April has an average temperature in the seventies, and by May it is in the eighties. And yet our containment efforts were so robust that the virus’s inflection point came before any seasonal trends, if they existed, could show themselves in full.
The end of sars was accompanied by a curious combination of hope and fatigue. We had been living indoors, secluded, behind masks, for so long that at some point it had become normal—even boring. I can remember the first time I saw someone wearing a mask, at the start of the outbreak: I had been taking my three-year-old daughter for a walk around Victoria Peak, and she had pointed him out. But I can’t remember when I first saw someone without one, or when I myself decided to leave mine at home. I suppose that, one day, I must have woken up, got dressed, reached for the N95 as usual, and then thought, Is this really necessary?
The government didn’t tell us to go out—and, in any case, it couldn’t have legislated away our fear. Instead, some internal calculation seemed to show that the benefits of living our lives newly outweighed the risks of catching sars. I know as I write this that it sounds ridiculous, but it felt as though the virus itself had grown weaker—as though it had been wounded. It seemed like a miasma had lifted from the city.
My family members came back from their exile. Restaurants reopened. The viral spell broke; Hong Kong seemed to wake from a fever dream. There were magical spring days when the sun flooded Victoria Harbor. We talked, in person. The virus had reduced everyone’s life to a binary—you either had it or you didn’t. Now, there seemed to be seven million different stories.
One day, I found myself sitting in a steamy chicken-and-rice place full of other customers. Oh, I thought. This is what life is.

Comments
Post a Comment